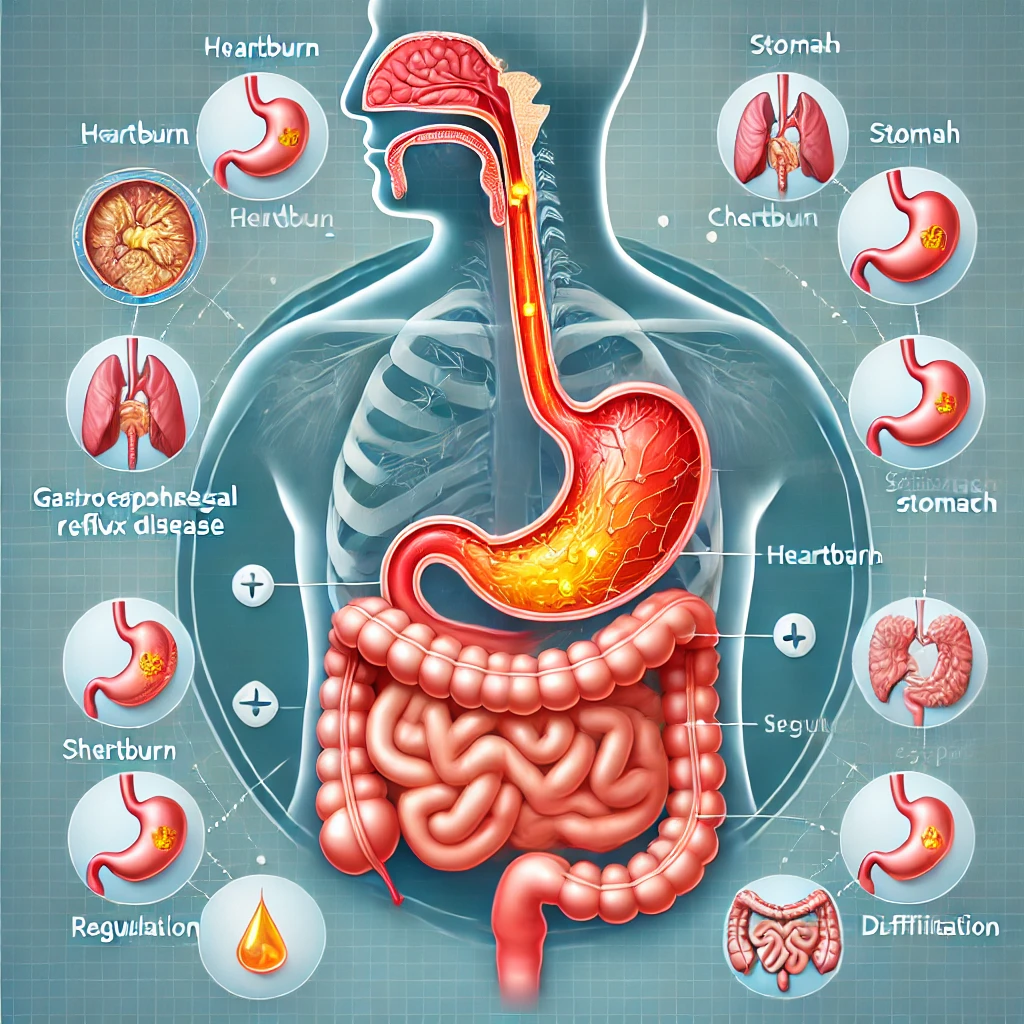
Gastroesophageal Reflux Disease (GERD) is a common yet often misunderstood digestive condition that affects millions of people worldwide. Characterized by chronic acid reflux, GERD occurs when stomach acid flows back into the esophagus, causing discomfort and potential complications. In this blog post, we’ll explore what GERD is, its causes, symptoms, and treatment options, as well as tips for managing the condition effectively.
What Is GERD?
GERD is a chronic digestive disorder where the lower esophageal sphincter (LES) — a muscular ring that acts as a valve between the esophagus and stomach — becomes weak or relaxes abnormally. This allows stomach acid and partially digested food to flow back into the esophagus, leading to symptoms such as heartburn and regurgitation. While occasional acid reflux is normal, GERD is diagnosed when it occurs frequently, typically more than twice a week.
Causes of GERD
Several factors can contribute to the development of GERD:
- Weak or Relaxed LES: When the LES doesn’t close properly, it allows acid to escape into the esophagus.
- Hiatal Hernia: A condition where part of the stomach pushes through the diaphragm, weakening the LES.
- Obesity: Excess weight increases pressure on the abdomen, pushing stomach contents into the esophagus.
- Dietary Choices: Foods like spicy dishes, citrus fruits, chocolate, caffeine, alcohol, and fatty meals can trigger reflux.
- Smoking: Smoking weakens the LES and reduces saliva production, which helps neutralize acid.
- Pregnancy: Hormonal changes and increased abdominal pressure can lead to GERD during pregnancy.
- Medications: Certain drugs, such as pain relievers, sedatives, or calcium channel blockers, can relax the LES.
Symptoms of GERD
GERD symptoms can vary in severity and frequency. The most common symptoms include:
- Heartburn: A burning sensation in the chest, often after eating or when lying down.
- Regurgitation: A sour or bitter-tasting acid or food backing up into the throat or mouth.
- Chest Pain: Discomfort that may mimic the symptoms of a heart attack.
- Difficulty Swallowing (Dysphagia): A feeling of food being stuck in the throat or chest.
- Chronic Cough: Persistent coughing caused by acid irritating the throat and airways.
- Hoarseness or Sore Throat: Acid reflux can inflame the vocal cords and throat.
- Nausea or Vomiting: Some individuals may experience digestive upset or vomiting after meals.
Potential Complications of GERD
If left untreated, GERD can lead to more serious health issues that go beyond the uncomfortable symptoms of heartburn and regurgitation. Over time, the persistent backflow of stomach acid into the esophagus can cause inflammation and damage to the delicate lining of the esophagus, a condition known as esophagitis. This inflammation can result in painful swallowing and increased sensitivity in the esophagus. In some cases, chronic acid exposure can lead to the formation of esophageal strictures, which are narrowings caused by scar tissue. These strictures can make swallowing difficult and uncomfortable, potentially interfering with proper nutrition.
One of the more concerning complications of untreated GERD is Barrett’s esophagus, a condition where the cells lining the esophagus change in response to repeated acid exposure. Barrett’s esophagus is considered a precancerous condition and can increase the risk of developing esophageal cancer, although the progression to cancer is rare.
Additionally, GERD can have effects outside the digestive system. Respiratory problems such as chronic cough, asthma-like symptoms, and even aspiration pneumonia may develop due to acid reflux reaching the throat and lungs. Laryngitis or chronic hoarseness can also occur if stomach acid irritates the vocal cords over time.Because of these potential risks, early diagnosis and effective management of GERD are essential to preventing long-term damage and improving overall quality of life.
- Esophagitis: Inflammation of the esophagus caused by prolonged acid exposure.
- Esophageal Strictures: Narrowing of the esophagus due to scar tissue, making swallowing difficult.
- Barrett’s Esophagus: A condition where the lining of the esophagus changes, increasing the risk of esophageal cancer.
- Respiratory Issues: GERD can worsen asthma or lead to chronic bronchitis, laryngitis, or aspiration pneumonia.
Diagnosing GERD
If you experience persistent symptoms, a healthcare provider may use the following methods to diagnose GERD:
- Medical History and Physical Exam: Discussing your symptoms and lifestyle habits.
- Endoscopy: A thin, flexible tube with a camera is used to examine the esophagus and detect inflammation or damage.
- pH Monitoring: Measures acid levels in the esophagus over 24 hours to confirm reflux.
- Esophageal Manometry: Assesses the function of the LES and esophageal muscles.
- Barium Swallow: X-rays taken after swallowing a contrast solution to detect abnormalities.
Treatment Options for GERD
Effective GERD management often involves a combination of lifestyle changes, medications, and, in severe cases, surgical intervention.
1. Lifestyle Modifications
- Dietary Changes: Avoid trigger foods like spicy, acidic, or fatty meals. Eat smaller, more frequent meals instead of large portions.
- Weight Management: Losing excess weight can reduce abdominal pressure and alleviate symptoms.
- Elevate the Head During Sleep: Raising the head of your bed by 6–8 inches helps prevent nighttime reflux.
- Quit Smoking: Smoking weakens the LES and increases acid production.
- Avoid Lying Down After Meals: Wait at least 2–3 hours after eating before lying down or going to bed.
2. Medications
- Antacids: Over-the-counter remedies that neutralize stomach acid (e.g., Tums, Rolaids).
- H2 Receptor Blockers: Reduce acid production (e.g., ranitidine, famotidine).
- Proton Pump Inhibitors (PPIs): Stronger medications that block acid production and heal the esophagus (e.g., omeprazole, lansoprazole).
- Prokinetics: Help strengthen the LES and speed up stomach emptying (e.g., metoclopramide).
3. Surgical Treatments
For severe GERD that doesn’t respond to lifestyle changes or medications, surgery may be an option:
- Fundoplication: The upper part of the stomach is wrapped around the LES to strengthen it and prevent reflux.
- LINX Device: A magnetic ring implanted around the LES to help it close properly.
Tips for Managing GERD
- Keep a Food Diary: Track your meals to identify and avoid trigger foods.
- Chew Slowly: Eating slowly and chewing thoroughly can reduce pressure on the stomach.
- Stay Hydrated: Drink plenty of water, but avoid drinking large amounts during meals.
- Wear Loose Clothing: Tight clothes can increase abdominal pressure and worsen reflux.
- Seek Medical Advice Early: Don’t ignore persistent symptoms; early treatment can prevent complications.
When to See a Doctor
If you experience severe or frequent symptoms, such as difficulty swallowing, unexplained weight loss, or chest pain, consult a healthcare provider immediately. GERD is a manageable condition, but timely intervention is crucial for preventing long-term complications.
Conclusion
GERD is a chronic but treatable condition that can significantly impact quality of life if left unmanaged. By understanding its causes and symptoms and making simple lifestyle changes, you can reduce discomfort and improve your digestive health. With the right treatment plan and proactive care, most individuals with GERD can lead a healthy and comfortable life. If you suspect you may have GERD, don’t hesitate to consult a gastroenterologist for a comprehensive evaluation and personalized treatment plan. Your digestive health is worth the attention!